Melanomas not only originate on the skin (in many cases they arise from a pre-existing mole), but also in the mucous and in the eye.
Cutaneous melanomas originate on intact skin or from preexisting, congenital or acquired moles.
It is a particularly aggressive type of cancer with 7,000 recorded new cases and 1,500 deaths each year in Italy.
It affects mostly middle-aged people (average of 57 years at diagnosis, 67 years to their death); 20% of cases are unfortunately individuals between 15 and 39 years of age.
RISK FACTORS
- individual factors
– family history of melanoma
– personal history of melanoma
– skin phenotypic factors: light, red or blond hair; blue eyes; freckles
– presence of a high number of moles (> 50); congenital and atypical moles
– prior sunburn
– Genetic diseases: xeroderma pigmentosum
– immunosuppression
– PUVA therapy
- Environmental factors related to lifestyle
– over exposure to sunlight
– over exposure to artificial radiation (sunbeds and tanning lamps)
– Insufficient sunscreen protection for long exposures
SIGNS AND SYMPTOMS
The main symptom is the change in the appearance of a mole or the appearance of a new one. The morphological aspects to be assessed are summarized by the acronym ABCDE
A Asymmetry-> shape irregularities: one half of the mole is different
B Borders-> irregular, jagged edges
C Colour-> dark or uneven with shades within the same mole
D Dimension-> greater than 6 mm in diameter
E Evolution-> elevation, extension, spontaneous bleeding independent of any trauma
PRIMARY PREVENTION AND EARLY DETECTION
The prevention of this disease, with an incidence rate that varies from 12 to 20 cases a year per 100,000 inhabitants, is the only truly effective weapon in fighting it.
Primary prevention aims at reducing incidences of cancer by removing the causes that give rise to it and is carried out by primarily avoiding over exposure to natural ultraviolet radiation (sun) and artificial radiation (tanning beds).
Sun exposure during the hottest hours without protection of hats and sunscreen is strongly discouraged. It is especially important to avoid sunburn at a young age.
Excessive exposure to the sun, as well as being the most important factor of skin aging, also encourages the development of other skin cancers such as basal cell and squamous cell carcinomas particularly common among people who have spent years and years in the sun (farmers and fishermen).
Lighter skin types are most affected, yet also the typical Mediterranean population, (with dark hair and skin) are not immune to risks and should still protect themselves.
Secondary prevention is aimed at early detection of suspicious or malignant lesions through periodic dermatologic check-ups with the help of a dermoscopy.
Most moles are not dangerous, but some have characteristics very similar to those of a melanoma. Atypical or dysplastic moles are fairly common and usually have a diameter greater than 6 mm, a variegated color, indistinct edges and sometimes a noticeable central papule and a “fried egg” look. A patient with atypical moles have an increased risk even in the absence of a personal and family melanoma history.
Dermatoscopy (also known as dermoscopy, epiluminesence microscopy) is a dermatological non-invasive method that allows you to examine the characteristics of epidermal pigmented structures, unnoticeable to a simple inspection with the naked eye. The survey facilitates the diagnosis and reduces the need to resort to biopsies for diagnostic purposes.
The observation is made by placing the instrument optics directly on the skin. There are two versions:
- the manual dermatoscope with a magnifying glass of 10-20 fold magnification and a light that allows the illumination of the skin surface to be examined
- A digital videodermatoscope not only permits viewing examined lesions on a monitor, but also various types of image processing, the storage of the image itself and their comparison over successive visits.
The method consists of applying a drop of colorless liquid (e.g. Mineral oil, ultrasound gel, or simply a drop of water) on the lesion to be examined and supporting the lens of the device on it. At this point, thanks to the liquid’s ability to cancel the reflective power of the epidermal corneous layer, you are able to view the morphological aspects of the lesion that allow you to provide a more accurate diagnosis.
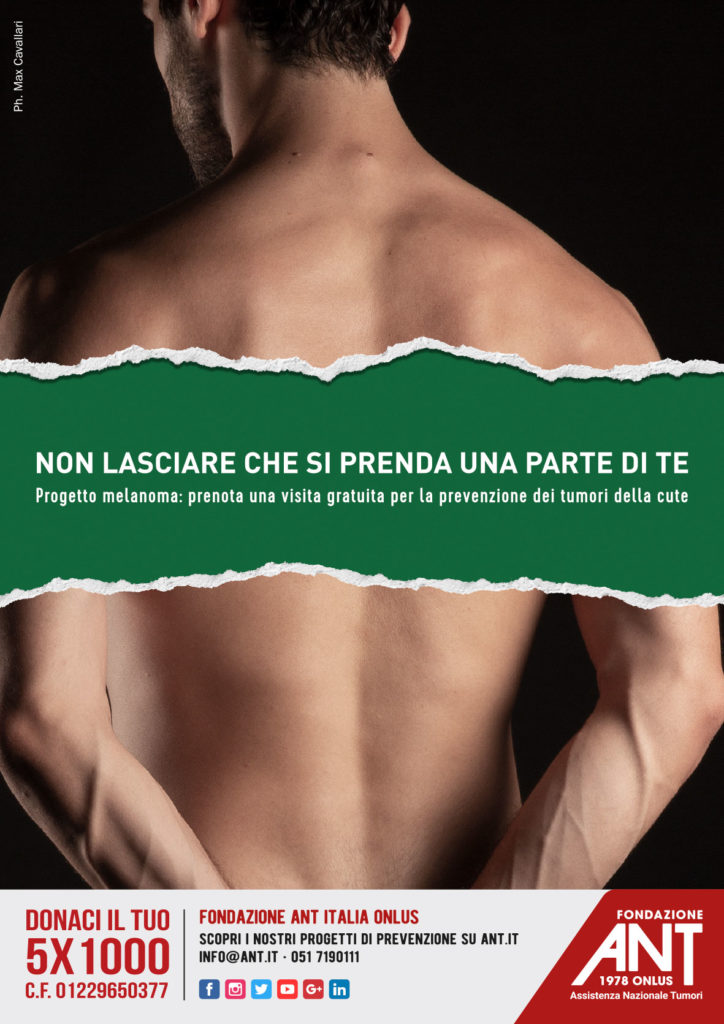
The ANT MELANOMA PROJECT provides for the execution of dermatological visits with the aid of a videodermatoscope. Check-ups (offered for free and by appointment thanks to funds / resources / donations that the Foundation is able to devote to this sector) are performed at the following clinics:
- the ANT Institute in Bologna
- the ANT delegations in Brescia, Pesaro, Porto S. Elpidio
- around the country offered for free by ANT